Cranial nerves are 12 pairs of nerves originating from the brain, controlling vital functions like sensory input and motor responses. They play a crucial role in neurological examinations, diagnosing various conditions by assessing their function.
1;1 Overview of Cranial Nerves
Cranial nerves are 12 pairs of vital nerves originating from the brainstem, responsible for controlling sensory, motor, and parasympathetic functions. They regulate essential processes like vision, hearing, smell, taste, and facial movements. Each nerve has specific roles, such as the olfactory nerve for smell and the optic nerve for vision. Damage to these nerves can result in deficits like blindness, hearing loss, or facial paralysis. Their unique pathways and functions make them critical for diagnosing neurological conditions, emphasizing the importance of thorough examination techniques in clinical practice.
1.2 Importance of Cranial Nerve Examination
Cranial nerve examination is a cornerstone of neurological assessment, providing critical insights into brain function and peripheral nervous system integrity. It helps diagnose conditions like stroke, multiple sclerosis, or nerve lesions by identifying deficits in sensory or motor functions. Early detection of abnormalities can guide timely interventions, improving patient outcomes. While often perceived as complex, its significance in localizing neurological damage and tailoring treatment plans makes it indispensable in clinical practice. Accurate assessment of cranial nerves ensures comprehensive evaluation of nervous system health.
Anatomy of Cranial Nerves
Cranial nerves originate from the brainstem, controlling sensory, motor, and parasympathetic functions. They consist of 12 pairs, each with unique pathways and roles in bodily operations.
2.1 Structure and Function of Cranial Nerves
Cranial nerves are composed of sensory, motor, or mixed fibers, each serving distinct functions. Sensory nerves transmit information like smell or vision, while motor nerves control muscle movements. Mixed nerves, such as the trigeminal, combine both roles. Their structure includes axons bundled in Schwann cells, protected by meninges. Functions range from regulating eye movements to controlling taste and hearing. Understanding their anatomy aids in diagnosing neurological disorders during examinations.
2.2 Classification of Cranial Nerves
Cranial nerves are categorized based on their functions: sensory, motor, or mixed. Sensory nerves, like the optic and olfactory, transmit sensory information. Motor nerves, such as the oculomotor and facial, control muscle movements. Mixed nerves, like the trigeminal, combine both sensory and motor roles. This classification aids in understanding their roles and identifying dysfunction during examinations. Accurate classification is crucial for diagnosing neurological conditions and tailoring treatment plans effectively.
2.3 Cranial Nerve Pathways and Innervation
Cranial nerves originate from the brainstem and traverse specific pathways to innervate target tissues. Each nerve has a unique course, such as the trigeminal nerve branching into ophthalmic, maxillary, and mandibular divisions. These pathways determine their functional roles, whether sensory, motor, or mixed. For instance, the oculomotor nerve controls eye movements, while the vagus nerve innervates visceral organs. Understanding these pathways is essential for localizing lesions and diagnosing neurological deficits. Accurate knowledge of their innervation patterns aids in correlating clinical findings with specific nerve dysfunction.

Clinical Significance of Cranial Nerve Examination
Cranial nerve examinations are vital for assessing neurological function, identifying nerve damage, and guiding treatment plans, playing a crucial role in diagnosing various neurological conditions accurately.
3.1 Common Indications for Cranial Nerve Testing
Cranial nerve testing is commonly indicated for patients presenting with symptoms like vision loss, facial weakness, or impaired sensory function. It is essential for diagnosing conditions such as multiple sclerosis, stroke, or nerve lesions. Testing is also warranted in cases of head trauma, infections, or tumors affecting the brain or skull. Additionally, cranial nerve assessment is crucial for evaluating swallowing difficulties, hearing loss, or olfactory disturbances. It serves as a critical tool in neurological exams to identify abnormalities and guide appropriate treatment plans, ensuring comprehensive patient care.
3.2 Role in Neurological Diagnosis
Cranial nerve examination plays a pivotal role in neurological diagnosis by providing insights into brain function and identifying specific nerve impairments. It helps localize lesions, differentiate between central and peripheral nervous system disorders, and assess the severity of neurological conditions. Cranial nerve testing is integral for diagnosing conditions like multiple sclerosis, stroke, and peripheral neuropathies. By evaluating nerve function, clinicians can monitor disease progression and response to treatment, ensuring accurate and timely interventions. This examination is a cornerstone in neurology, offering a detailed understanding of the nervous system’s integrity and functional status.
Preparing for Cranial Nerve Examination
Proper patient preparation involves positioning, ensuring a calm environment, and having essential tools ready for a thorough assessment of cranial nerve function and neurological responses.
4.1 Patient Preparation and Positioning
Patient preparation is crucial for an effective cranial nerve examination. Ensure the patient is comfortable and positioned appropriately, with good lighting for visual assessments. For specific nerves, such as the optic (CN II) and vestibulocochlear (CN VIII), certain positions may enhance testing accuracy. Instruct the patient to remove eyewear or hearing aids if necessary. A quiet, distraction-free environment is ideal for evaluating nerves like the olfactory (CN I) and trigeminal (CN V). Proper positioning and clear instructions help maximize the reliability of the examination findings.
4.2 Essential Tools and Equipment
The cranial nerve examination requires specific tools to ensure accuracy. A penlight is used for assessing pupil reactions and visual fields. An ocular funduscope or ophthalmoscope helps examine the optic nerve. A tuning fork or audiometer is essential for testing hearing (CN VIII). A cotton swab or feather tests sensory function for CN V, while a tongue depressor aids in assessing CN IX and XII. A mirror or flashlight is used for observing facial symmetry (CN VII). These tools, along with standard medical equipment, are indispensable for a comprehensive evaluation of cranial nerve function.

Examination Techniques for Cranial Nerves
Systematic assessment of each cranial nerve employs specific tests to evaluate sensory, motor, and reflex functions, ensuring accurate neurological evaluation and diagnosis of potential abnormalities.
5.1 Testing Cranial Nerve I (Olfactory Nerve)
Testing Cranial Nerve I involves assessing the sense of smell. The patient is asked to identify specific odors, such as vanilla or peppermint, using each nostril separately. This evaluates the nerve’s ability to transmit sensory information from the olfactory receptors in the nasal mucosa to the brain. Bilateral testing ensures comparison of olfactory function between the two sides. Reduced or absent smell sensation may indicate nerve damage or conditions like anosmia, providing critical clues for neurological diagnostics and further investigation.
5.2 Assessing Cranial Nerve II (Optic Nerve)
Assessment of Cranial Nerve II involves evaluating visual function. Visual acuity is tested using a Snellen chart to measure central vision. Pupil reactions, including the direct and consensual light reflex, are examined to assess autonomic function. Visual field testing, such as confrontation testing, identifies defects in peripheral vision. Abnormalities may indicate conditions like optic neuritis or pituitary tumors. Accurate documentation of findings is crucial for diagnosing neurological or ophthalmological disorders, making this a cornerstone of cranial nerve examinations.
5.3 Evaluating Cranial Nerve III (Oculomotor Nerve)
Evaluation of the oculomotor nerve involves assessing its control over eye movements, pupil constriction, and eyelid elevation. Clinicians test eye movements by asking the patient to follow a moving object in all directions. The pupillary light reflex is examined by shining a light into each eye to observe pupil constriction. Ptosis, or eyelid drooping, is noted if the levator palpebrae superioris muscle is impaired. Abnormalities may include anisocoria or impaired extraocular muscle function, potentially indicating conditions like third cranial nerve palsy. Accurate assessment requires attention to these specific functions.
5.4 Examining Cranial Nerve IV (Trochlear Nerve)
The trochlear nerve, the fourth cranial nerve, controls the superior oblique muscle, which rotates the eye downward and inward. Examination involves assessing this muscle’s function. The patient is asked to look downward while the head is tilted forward. The examiner checks for smooth, coordinated eye movement and absence of ptosis. Weakness or paralysis of the superior oblique muscle may indicate a trochlear nerve lesion, often presenting as difficulty moving the affected eye downward. This test is crucial for identifying issues related to the trochlear nerve’s specific motor function.
5.5 Testing Cranial Nerve V (Trigeminal Nerve)
The trigeminal nerve, the fifth cranial nerve, is the largest and has three divisions: ophthalmic, maxillary, and mandibular. Sensory function is tested by lightly touching the face with a soft object and assessing pain sensation with a pin. Motor function is evaluated by examining the muscles of mastication, such as the temporalis and masseter, during jaw clenching. Weakness or sensory loss may indicate nerve damage or conditions like trigeminal neuralgia. This nerve is crucial for facial sensation and chewing, making its examination essential for diagnosing various neurological disorders.
5.6 Assessing Cranial Nerve VI (Abducens Nerve)
Cranial Nerve VI, the abducens nerve, controls lateral eye movement via the lateral rectus muscle. To assess its function, ask the patient to look laterally in both directions. Observe for weakness or paralysis of eye abduction. If damaged, the eye may turn medially due to unopposed medial rectus muscle action. This nerve is commonly affected in conditions like increased intracranial pressure or lesions in the brainstem or orbit. Accurate testing is essential for diagnosing abnormalities in eye movement and related neurological conditions.
5.7 Evaluating Cranial Nerve VII (Facial Nerve)
Cranial Nerve VII, the facial nerve, controls facial expressions, taste sensation in the anterior tongue, and parasympathetic functions. Examination involves assessing facial symmetry and strength by having the patient smile, frown, close eyes tightly, and puff cheeks. Taste can be tested using sweet, sour, salty, and bitter substances. Look for unilateral weakness, which may indicate Bell’s palsy or other pathologies. Accurate evaluation helps diagnose conditions affecting the nerve, ensuring appropriate management and treatment.
5.8 Examining Cranial Nerve VIII (Vestibulocochlear Nerve)
Cranial Nerve VIII, the vestibulocochlear nerve, is responsible for hearing and balance. Examination involves assessing hearing with tests like pure tone audiometry and speech recognition. Vestibular function is evaluated using caloric reflex testing, which involves irrigating the ears with warm or cold water to elicit nystagmus. Abnormal findings may indicate conditions such as Meniere’s disease, acoustic neuromas, or labyrinthitis. Accurate assessment of this nerve is critical for diagnosing auditory and vestibular disorders, ensuring proper management and rehabilitation strategies.
5.9 Testing Cranial Nerve IX (Glossopharyngeal Nerve)
Cranial Nerve IX, the glossopharyngeal nerve, is tested by assessing taste sensation, swallowing, and salivation. Taste is evaluated using sweet or sour substances applied to the posterior tongue. The gag reflex is checked by gently stimulating the pharynx with a cotton swab. Observation of the uvula’s elevation during swallowing is also performed. Abnormalities may indicate issues like dysphagia or neurological dysfunction. This nerve’s examination is vital for diagnosing conditions affecting swallowing and taste, ensuring proper management of related disorders.
5.10 Assessing Cranial Nerve X (Vagus Nerve)
Cranial Nerve X, the vagus nerve, is assessed by evaluating functions such as swallowing, voice quality, and the gag reflex. The patient is asked to swallow, and the examiner observes the movement of the pharynx and uvula. The gag reflex is tested by stimulating the pharyngeal wall with a cotton swab. Abnormalities may indicate issues like dysphonia or dysphagia. Additionally, the examiner may check for hoarseness, which could suggest nerve dysfunction. This nerve’s examination is critical for identifying conditions affecting swallowing and voice production.
5.11 Evaluating Cranial Nerve XI (Accessory Nerve)
Cranial Nerve XI, the accessory nerve, is evaluated by assessing the strength and function of the sternocleidomastoid and trapezius muscles. The patient is asked to shrug their shoulders and rotate their head against resistance. The examiner observes for muscle atrophy, weakness, or fasciculations. Palpation of the muscles may reveal tenderness or abnormal contractions. Normal function indicates intact motor pathways, while deficits may suggest nerve damage or underlying neurological conditions. This nerve’s examination is essential for diagnosing issues related to neck movement and shoulder stability.
5.12 Examining Cranial Nerve XII (Hypoglossal Nerve)
Cranial Nerve XII, the hypoglossal nerve, is assessed by evaluating tongue movements and strength. The patient is asked to protrude their tongue, move it side to side, and push against the examiner’s finger. The examiner observes for tongue deviation, atrophy, or fasciculations. Speech is also evaluated for articulation difficulties. Normal function indicates intact motor control, while weakness or irregular movements may suggest nerve damage or neurological disorders. This examination is critical for identifying issues affecting speech and swallowing functions.

Documenting Cranial Nerve Examination Findings
Accurate documentation of cranial nerve examination findings is essential for tracking patient progress and diagnosis. Findings are recorded using standardized formats, noting abnormalities and test results clearly.
6.1 Recording Observations and Results
During cranial nerve examination, observations and results are meticulously recorded to ensure clarity and accuracy. Standardized formats, such as checklists or narrative descriptions, are used to document findings. Abnormalities, such as weakness or sensory deficits, are highlighted. Results from tests like visual acuity, pupillary responses, and muscle strength are included. This documentation serves as a reference for future comparisons and facilitates communication among healthcare providers. Detailed records help in tracking patient progress and informing diagnostic or therapeutic decisions.
6.2 Interpreting Abnormal Findings
Abnormal findings during cranial nerve examination require careful interpretation to identify underlying pathologies. Lesions or dysfunction in specific nerves can indicate localized or systemic conditions. For instance, unilateral weakness in cranial nerve VII (facial nerve) may suggest a stroke or Bell’s palsy. Abnormal pupillary responses could signify optic nerve damage or autonomic dysfunction. Correlating findings with patient symptoms and medical history is essential for accurate diagnosis. Further diagnostic tests, such as imaging or electromyography, may be recommended to confirm the cause of abnormalities. Timely interpretation ensures appropriate management and improves patient outcomes.

Common Pathologies and Cranial Nerve Involvement
Common pathologies involving cranial nerves include, for example, Bell’s palsy affecting the facial nerve (CN VII), multiple sclerosis, brainstem strokes, and trigeminal neuralgia impacting CN V.
7.1 Cranial Nerve Lesions and Their Implications
Cranial nerve lesions involve damage to one or more cranial nerves, often due to trauma, tumors, infections, or vascular disorders. These lesions can lead to specific deficits, such as vision loss (CN II), facial weakness (CN VII), or impaired swallowing (CN IX and CN X). Early identification of lesions through detailed neurological examination is critical for targeted treatment and improving patient outcomes. Lesions in cranial nerves provide valuable diagnostic clues about underlying conditions, such as multiple sclerosis or brainstem pathologies, emphasizing their clinical significance in neurological care.
7.2 Neurological Conditions Associated with Cranial Nerve Dysfunction
Cranial nerve dysfunction is linked to various neurological conditions, including multiple sclerosis, stroke, brain tumors, and Guillain-Barré syndrome. These conditions often manifest through specific deficits, such as diplopia (CN III, IV, VI) or facial paralysis (CN VII). Cranial nerve involvement can also indicate systemic diseases like Lyme disease or diabetes. Early detection of dysfunction through thorough examination aids in diagnosing these conditions, guiding timely interventions. Recognizing patterns of cranial nerve impairment is essential for accurate neurological assessment and effective patient management, highlighting their role as critical diagnostic tools in clinical practice.
Special Considerations in Cranial Nerve Examination
Cranial nerve exams require tailored approaches for pediatric and geriatric patients, as well as unconscious individuals. Techniques must adapt to age-related physiological changes and patient responsiveness to ensure accurate neurological assessment.

8.1 Pediatric and Geriatric Considerations
Cranial nerve examinations in pediatric and geriatric populations require special attention due to age-related physiological differences. In children, the examination must be adapted to their developmental stage, ensuring cooperation through age-appropriate techniques. Geriatric patients may present with age-related declines in sensory or motor function, necessitating careful differentiation between normal aging and pathological conditions. Additionally, in both groups, non-compliance or cognitive impairments may challenge the examination process, requiring patience and tailored approaches to accurately assess cranial nerve function and neurological status.
8.2 Examination of Unconscious Patients
Examining cranial nerves in unconscious patients requires a tailored approach, focusing on reflexes and involuntary responses. Pupillary reactions assess cranial nerves II and III, while corneal reflexes evaluate cranial nerves V and VII. The gag reflex tests cranial nerves IX and X. Observing eye movements and tongue symmetry helps assess cranial nerves III, IV, VI, and XII. These tests provide critical insights into neurological status, guiding diagnosis and treatment in non-responsive patients.
Cranial nerve examination remains a cornerstone in neurological assessment, offering insights into brain function and disorders. Future advancements in techniques and technologies promise enhanced diagnostic accuracy and patient care.
9.1 Summary of Key Points
Cranial nerve examination is a fundamental tool in neurology, providing critical insights into brain function and aiding in the diagnosis of various neurological conditions. The 12 cranial nerves control essential functions, from sensory perception to motor responses. Proper examination techniques, such as testing olfactory, optic, and motor functions, are vital for accurate diagnoses. Abnormal findings can indicate specific pathologies, making this assessment indispensable in clinical practice. By mastering cranial nerve evaluation, healthcare professionals can enhance patient care and improve outcomes in neurological disorders.
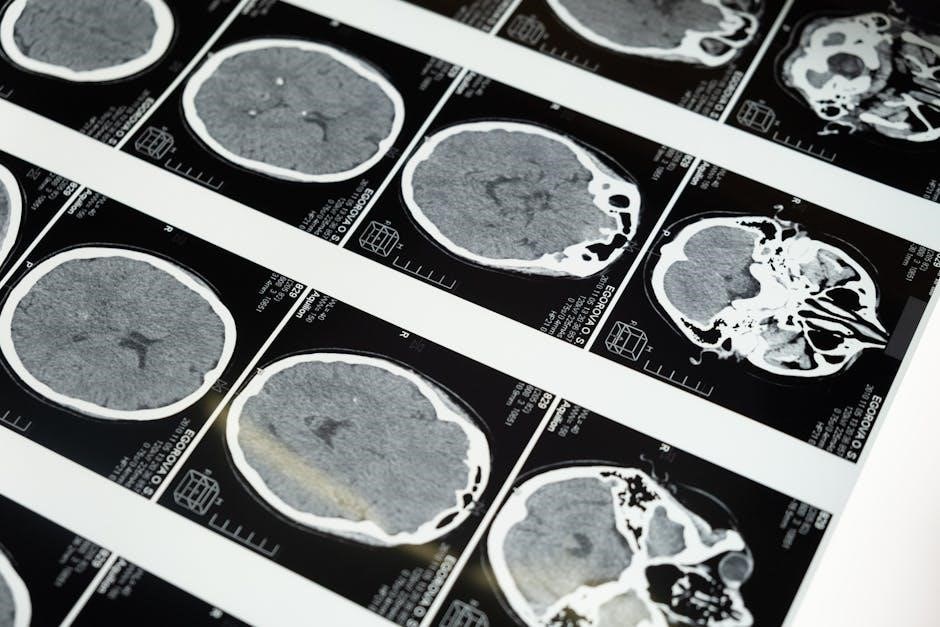
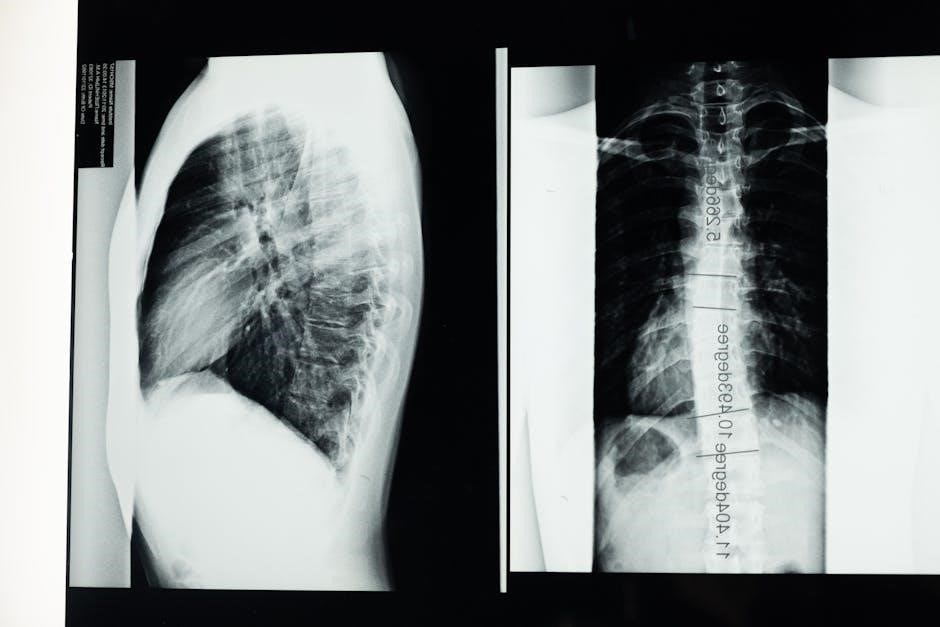
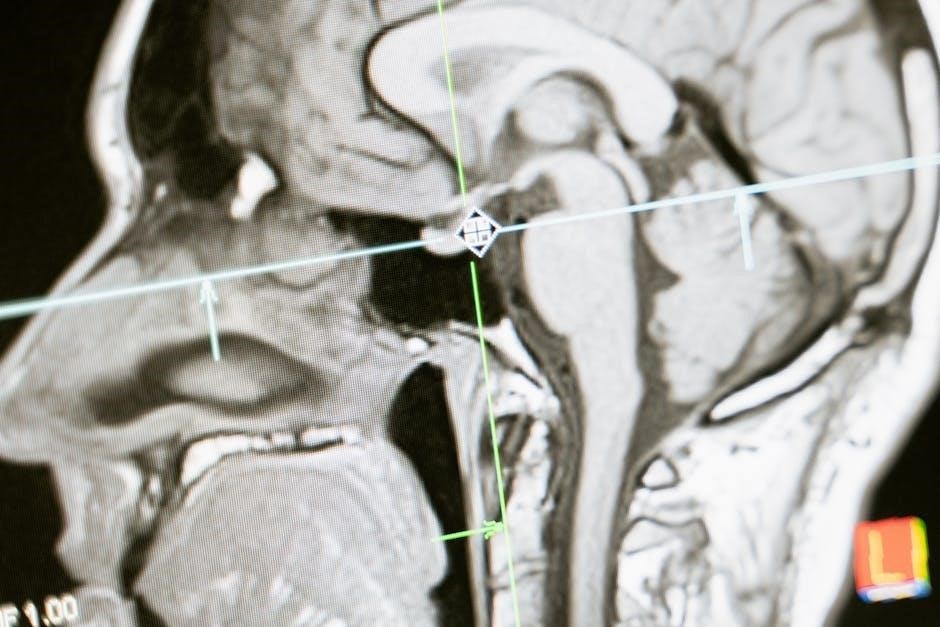
9.2 Advances in Cranial Nerve Examination Techniques
Recent advancements in cranial nerve examination techniques include the integration of advanced neuroimaging tools like MRI and CT scans for precise nerve visualization. Electrophysiological tests, such as nerve conduction studies, now offer deeper insights into nerve function. Additionally, the development of non-invasive methods, such as optical coherence tomography for optic nerve assessment, has enhanced diagnostic accuracy. These innovations improve early detection of abnormalities, enabling timely interventions and better patient outcomes. Continuous research focuses on refining examination protocols to ensure reliability and efficiency in clinical practice.